Blogs
Living with diabetes requires understanding, resilience, and a commitment to well-being, shaping a fulfilling life.

Guide for Everyday foot care for Diabetics
24.10.2023
In the second of our series on foot care, we’re looking specifically at how to look after your feet if you’re a diabetes sufferer.
Foot care is important for us all but, unfortunately, serious foot problems can be commonplace for diabetics and can, in extreme cases, lead to the need for amputation.
However, most amputations can be prevented with good, regular foot care and a mindful approach to reducing your risk of developing untreatable & serious foot conditions.
Why are diabetics prone to foot conditions?
Raised blood glucose (or blood sugar) levels are known to damage the sensation in your feet as well as affecting your circulation & blood supply to your extremities. Lack of decent blood supply in your feet can lead to cramps & pains, as well as slowing down the healing process on any cut or sores you might have.
If cuts and sores fail to heal, they could lead to ulcers, infections and in the worst case scenario to amputation.
So it’s imperative that diabetes patients look after their feet. Following these 5 top tips will put you on track to ensuring good foot health and keeping your feet and legs in tip top condition.
1) Check your feet every day
Because of your diabetes, foot problems can get worse quickly so early detection is really important.
Make a habit of checking for any cuts, sores, blisters or lack of feeling every morning or evening when you’re getting (un)dressed. If you spot any changes you should see a healthcare professional straight away.
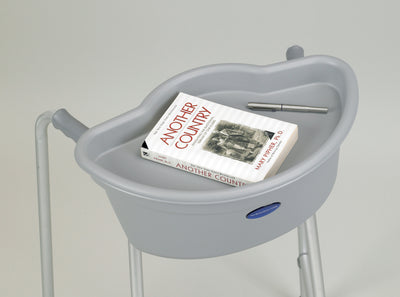
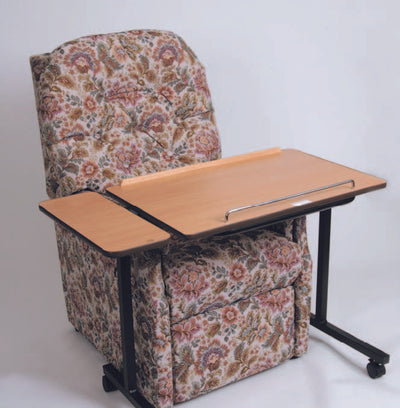
If you struggle to lift your feet up, then you might want to use a mirror to see the soles of your feet or try to get someone else to check your feet for you.
2) Manage your blood sugar levels, cholesterol and blood pressure
Keeping your blood sugar within target is important for diabetics anyway, but it’s vital for good foot health too. Fluctuating levels in blood sugar, cholesterol and blood pressure can all play havoc with the blood supply to your feet which can, in turn, lead to problems. Help prevent damage to your feet and stop things getting worse by managing your daily levels, and be sure to speak to your GP or consultant if you need support with this.
3) Be careful when cutting your toenails
Cutting your nails seems simple. But if you have diabetes, piercing the skin by mistake can lead to other injuries. Always use a proper nail clipper to cut your nails. If you struggle with your eyesight you might find a nail clipper with magnifying glass handy.
When you cut your toenails:
- cut them often but not too short or down the side
- trim them with nail clippers and then use an emery board to file any corners
- clean them gently with a nail brush - don’t use the sharp points of scissors to clean as this isn’t safe.
4) Keep Foot Washing Simple
Washing your feet daily is a very easy way to keep your feet and toenails clean, in check and away from infection. There’s no need to use fancy toiletries, in fact a simple mix of soap and warm water is more than sufficient.
It’s best not to soak your feet for long periods or to use very hot water as this softens the skin, makes it wrinkly/soggy and more likely to get damaged.
If you’ve lost some sensation in your feet or you’re worried about things like ingrown toenails, see a foot specialist. Do NOT try to fix issues like this yourself.
5) Avoid blades or corn plasters
Like everybody else, you might find that you develop a corn or rough skin on your feet. This is normal, but it’s also important that you don’t try to tackle sorting it yourself. Don’t use plasters to remove corns or blades on your corns or tough skin as they could damage your skin. Pumice stones can also help with tough skin, but do use them with care. Essentially you need to do what you can to avoid splitting the skin.
If you’re in any way unsure, you should always speak to a podiatrist.
Need more help with footcare? We're always here to help so get in touch today.
For all your Medical and Homecare supplies give us a call at Mediworld.
We have over 40 years experience in medical, surgical, mobility and home health supplies and we're always on hand to chat if you need support or advice. Follow us on Twitter and Facebook and don't forget to read our other great health blogs!
Learn More Now

Managing Diabetes and Insulin in Hot Weather
07.02.2024
We’re experiencing some really hot weather in the UK this summer, and for diabetics this can make managing blood sugar levels particularly tricky.
While lots of people are enjoying the warm sunshine, many diabetics will need to change their approach to controlling their glucose levels and how they store insulin when the temperature starts to rise.
Thankfully there’s some great advice from charities like Diabetes UK and Diabetes Org UK and with careful management anyone who suffers from Diabetes can, in fact, safely enjoy the heat and the sun this summer.
Why the heat affects blood sugar levels
There are actually several ways that heat can adversely affect blood sugar levels, insulin needs and even the vials of insulin themselves.
Heat: Whether it’s dry or humid, heat can quickly impact your hydration levels and cause your glucose levels to spike rapidly. Dehydration creates a situation where there is less fluid in your tissue and bloodstream, and therefore the glucose levels in the blood become more concentrated.
While activity is often associated with a change in sugar levels, just sitting still in the sun when it’s hot will cause a significant rise in blood sugar levels.
Sun Exposure: Sunburn, in particular, is incredibly stressful to the body. Sunburn is essentially a cellular inflammation which the body reacts to by producing more hormones, including cortisol, to manage and heal it. This can cause a spike in sugar levels and even temporary resistance to insulin for several days before it settles down.
How heat affects insulin intake
Heat affects both the effect of insulin in your body and the efficacy of the product while it’s in the vial.
If you take insulin to treat your diabetes, be aware that it will be absorbed more quickly from injection in warmer weather, which can increase the risk of hypos. Keeping hydrated is one way of maintaining good glucose levels and you should always seek help/guidance from your GP/specialist on management of your insulin levels during the heat.
How heat affects insulin vials
Put simply, insulin vials that are exposed to heat above an average room temperature will die. The vials don’t even need to be in heat for long before they start to break down. Just one hour in 25 degrees celsius will cause the insulin to become ineffective.
Once the vials become warm they no longer provide the amount of insulin stated on the label and will leave you vulnerable and unsure of the levels you’ve administered into your body. If your vial looks cloudy, discoloured, has visible particles or you think it’s been overexposed to heat you should throw it away. It will almost definitely have lost its effectiveness and won’t keep your blood sugars from getting too high.
Therefore, it's absolutely paramount that you store your insulin at a steady, cool temperature to ensure it’s effective when you need it.
How to store insulin in hot weather
The ideal temperature to store your insulin vials, pens, and pumps is between 2 and 6 degrees celsius. Storing them in the fridge is ideal.
Never leave your insulin in the car or in a bag that’s next to a radiator or sitting in the heat. Within just 60 minutes the insulin will be ineffective.
Even wearing your pump too close to your body on a hot day or while you’re exercising can cause the insulin to deteriorate quite rapidly.
So, if you must leave your insulin in your bag or even in your car because you’re out and about or travelling, then you’ll need a good insulin storage solution to keep your medication at the right temperature.
Use an insulin cool bag or an ice pack cooler to protect it. If you already have an insulin or EpiPen storage/travel you should consider keeping it in a cool box with a cool ice pack inside.
Metres and Test Strips
Don’t forget to keep your blood glucose metre and glucose test strips away from the sun and heat as well. Extreme temperatures can also affect their efficacy so store them as close to normal room temperature as possible, and always keep them out of direct sunlight.
Unfortunately they cannot be refrigerated, as extreme temperatures will lead to misleading results.
Need more help? We're always here to help so get in touch today.
For all your Medical and Homecare supplies give us a call at Mediworld.
We have over 40 years experience in medical, surgical, mobility and home health supplies and we're always on hand to chat if you need support or advice and don't forget to read our other great health blogs!
August 2022
Learn More Now